
Newer technology involves using concentrated bone cells or stem cells either harvested from the patient or from a donor. These materials can add volume to the bone graft without the need to harvest more bone. Other materials, like synthetic bone graft extenders or processed bone (called demineralized bone matrix) may also be used in combination with the bone graft and/or BMP. BMP aids in bone growth and is naturally produced by the body. To aid in bony fusion, the surgeon may also use a “bone promoting substance” like bone morphogenic protein, or BMP. Depending on the type of surgery, bone from the hip may be removed through the same surgical incision or through a separate incision. Sometimes bone removed from the patient during the decompression portion of the surgery can be used as a graft other times, the bone is taken from the patient’s iliac crest (hip bone). The graft may come from a bone bank or it may be taken from the patient’s own body.


To fuse the vertebrae, the surgeon places new bone material, called bone graft, as a bridge between existing bones. Then the surgeon performs the spinal fusion through the retractor. Bone or disc sections removed during a minimally invasive decompression are extracted through the tubular retractors. This is often a decompression procedure, performed to relieve pressure on the spinal cord or surrounding nerves. If another minimally invasive procedure must be performed during the same operation, it is performed first. The surgeries also tend to rely more upon intraoperative radiographic imaging to guide the surgeon. In order to see the area, surgeons may use an operating microscope positioned at the top of the retractor, or an endoscope (thin tube with a camera and a light at the end) that passes down through the retractor into the body. Unlike in some traditional surgical procedures, in minimally invasive procedures, surgeons may have a limited view of the surgical area. Some surgical procedures require more than one retractor. An instrument called a tubular retractor holds the tunnel open while the surgeon works.

The dilators create a tunnel through these tissues down to the spinal column.
#Spine fusion skin
These are tubes of expanding diameter that move aside the muscles and other tissues located between the skin incision and the spine. The number, location, size, and shape of the incisions vary depending on the location of the problem and the approach the surgeon has selected.įor most types of minimally invasive spinal fusion, the surgeon uses instruments called tubular dilators. In minimally invasive surgery, the surgeon makes small incisions. In adults and children, minimally invasive spinal fusion is performed under general anesthesia, which means the patient is unconscious. This approach produces the least disruption to muscles, bones, and abdominal organs.
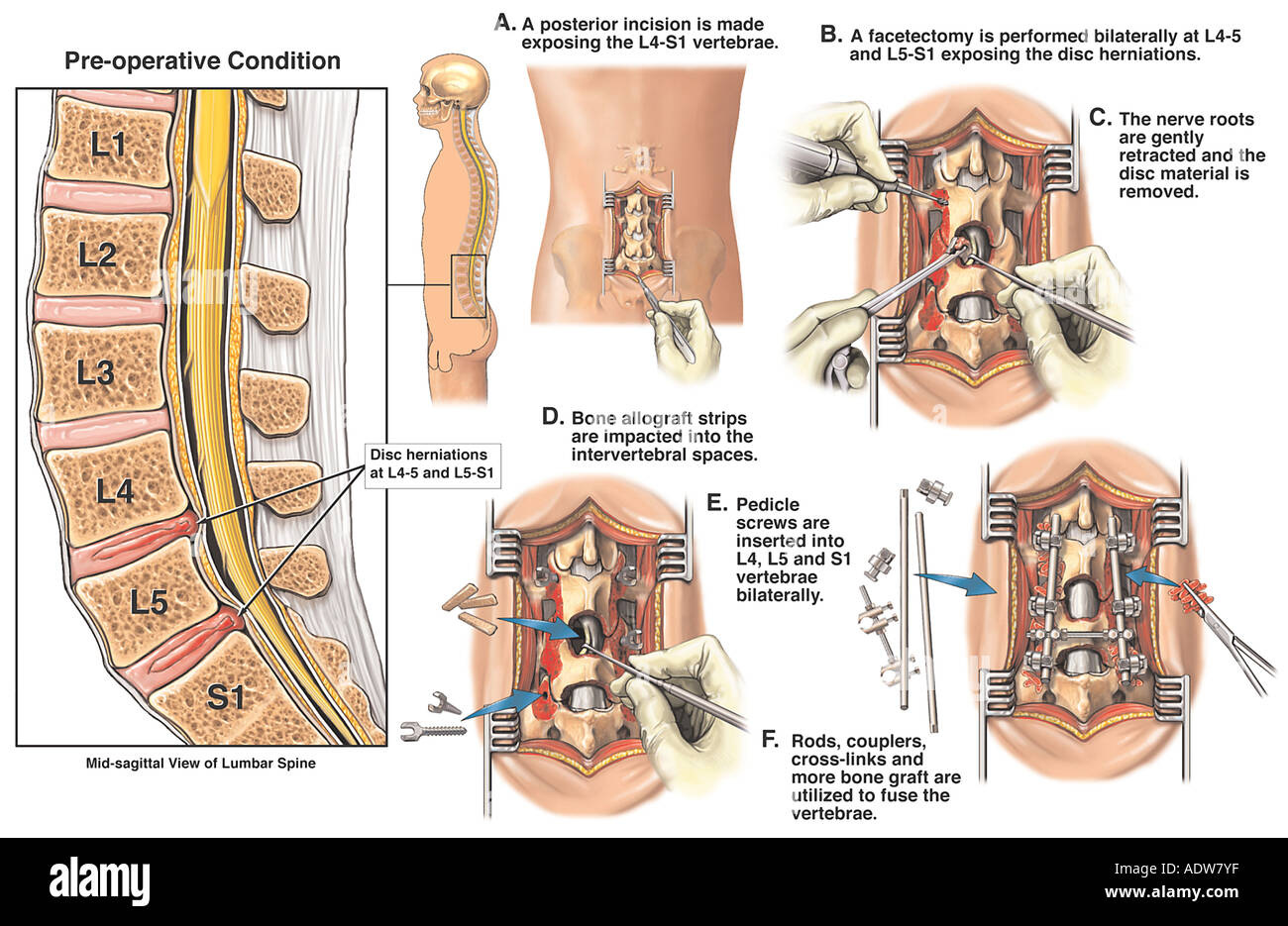
It is important to note that with any type of spine fusion, there is a risk of clinical failure (meaning that the patient's pain does not go away) despite achieving a successful fusion.Minimally invasive thoracic and lumbar fusion can be accomplished with the following procedures: Extreme lateral interbody fusion (XLIF) - an interbody fusion in which the approach is from the side.Transforaminal lumbar interbody fusion (TLIF) - Similar to the PLIF, this procedure is also done from the back of the spine.Anterior/posterior spinal fusion - the procedure is done from the front and the back.Anterior lumbar interbody fusion (ALIF) - the procedure is done from the front and includes removing the disc between two vertebrae and inserting bone into the space created between the two vertebral bodies.Posterior lumbar interbody fusion (PLIF) - the procedure is done from the back and includes removing the disc between two vertebrae and inserting bone into the space created between the two vertebral bodies.Posterolateral gutter fusion - the procedure is done through the back.The most commonly employed surgical techniques include: There are several types of spinal fusion surgery options.


 0 kommentar(er)
0 kommentar(er)
